Health
FODMAP made simple: the diet that’s changing gut health

A clear, no-nonsense guide to the FODMAP diet, what it actually does, and how it can help you finally figure out which foods your gut loves and which ones it would rather never see again.
By Sarah Coleman
If you often struggle with bloating, abdominal pain, diarrhoea, constipation or other ongoing digestive issues, the FODMAP diet may offer relief. Originally developed by researchers at Monash University here in Australia for people diagnosed with irritable bowel syndrome (IBS), studies show it may also help with other types of digestive discomfort.
Because it’s a structured, short-term plan designed to identify specific food triggers, it’s important to follow the FODMAP diet with support of a qualified dietitian or healthcare professional. That way, you can do it safely and get the most out of the process.
So, what are FODMAPs?
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. These are types of carbohydrates that can be difficult for some people to digest:
- Oligosaccharides - complex sugars found in foods like wheat, onions, garlic, beans and lentils.
- Disaccharides - mainly refers to lactose, the sugar in milk and dairy products such as yoghurt and cheese.
- Monosaccharides - include fructose in foods such as apples, pears, mangoes and honey.
- Polyols - also known as sugar alcohols (like sorbitol and mannitol), polyols are found naturally in fruits such as peaches and plums and are commonly added to many “sugar-free” foods.
When these carbohydrates reach your large intestine, gut bacteria ferment them, creating gas in the process. The buildup of gas and water causes the intestinal walls to expand. For people with IBS, whose guts are especially sensitive, this stretching can trigger stronger symptoms of pain, bloating and diarrhoea than in those without IBS.
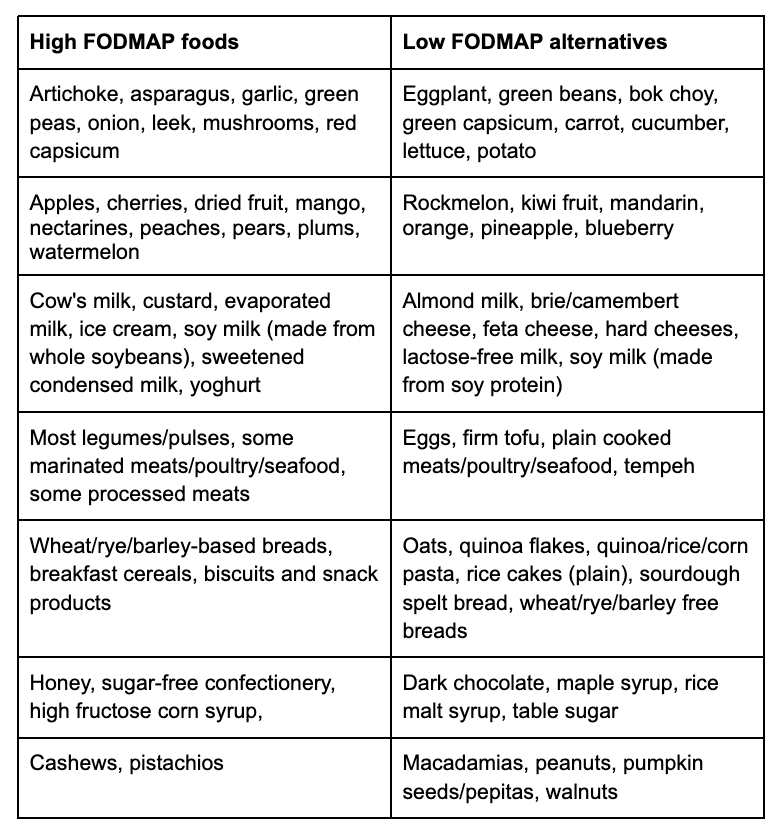
Which foods are high in FODMAPs?
As you can see from the list above, FODMAPs are found in many everyday foods, from fruits and vegetables to grains, legumes, dairy and processed products. This makes it hard to tell which foods are high or low in FODMAPs without expert guidance.
Here’s a brief overview:
High FODMAP foods
Low FODMAP alternatives
Artichoke, asparagus, garlic, green peas, onion, leek, mushrooms, red capsicum
Eggplant, green beans, bok choy, green capsicum, carrot, cucumber, lettuce, potato
Apples, cherries, dried fruit, mango, nectarines, peaches, pears, plums, watermelon
Rockmelon, kiwi fruit, mandarin, orange, pineapple, blueberry
Cow's milk, custard, evaporated milk, ice cream, soy milk (made from whole soybeans), sweetened condensed milk, yoghurt
Almond milk, brie/camembert cheese, feta cheese, hard cheeses, lactose-free milk, soy milk (made from soy protein)
Most legumes/pulses, some marinated meats/poultry/seafood, some processed meats
Eggs, firm tofu, plain cooked meats/poultry/seafood, tempeh
Wheat/rye/barley-based breads, breakfast cereals, biscuits and snack products
Oats, quinoa flakes, quinoa/rice/corn pasta, rice cakes (plain), sourdough spelt bread, wheat/rye/barley free breads
Honey, sugar-free confectionery, high fructose corn syrup,
Dark chocolate, maple syrup, rice malt syrup, table sugar
Cashews, pistachios
Macadamias, peanuts, pumpkin seeds/pepitas, walnuts
The three stages of the FODMAP diet
The FODMAP diet is typically completed under the guidance of a dietician or health professional and is divided into three phases:
Phase 1: Elimination (2-6 weeks)
In this first phase, you cut out all high FODMAPs foods and replace them with low FODMAP options. The goal is to calm your gut and reduce symptoms, think of it as a digestive “reset”.
Phase 2: Systematic Reintroduction (8-12 weeks)
Once symptoms ease, you begin adding FODMAP foods back into your diet one at a time, over several days each. This helps pinpoint which types of FODMAPs trigger your symptoms and how much you can tolerate. Some people find they only react to certain groups, while others can handle most foods in moderation.
Phase 3: Personalisation (Ongoing)
This final stage focuses on developing a sustainable, long-term eating plan. You reintroduce all foods you tolerate and only limit those that cause symptoms. The aim is to maintain a balanced, varied diet while managing digestive comfort and supporting long-term gut health.

Reality check
Not everyone with IBS responds to the FODMAP diet, which usually means that FODMAPs are not the main trigger for their symptoms. About 25% of people with IBS don’t experience significant improvement, and may need alternative treatments such as stress management, medications, or other dietary approaches.
The way the gut breaks down FODMAPs also varies from person to person. Each individual’s gut microbiome (the community of microbes living in the intestines) ferments carbohydrates differently, depending on the types and balance of microbes present.
Recent research suggests that a person’s unique gut microbiome may help predict how well they’ll respond to the FODMAP diet.
Also, strictly avoiding all high-FODMAP foods for long periods is not recommended. While short-term restriction can help calm gut symptoms, keeping these foods out of your diet for too long may lower important nutrient intake and reduce levels of beneficial gut microbes, particularly Bifidobacteria, which play a key role in maintaining a healthy microbiome.
Fortunately, studies show that once high-FODMAP foods are gradually reintroduced and the diet is personalised, gut microbe levels recover and overall gut health improves. This is why the reintroduction and personalisation stages of the diet are crucial for long-term success and digestive wellbeing.
Beyond IBS: emerging new uses for the FODMAP diet
Digestive symptoms like bloating, pain, and irregular bowel habits can occur in many health conditions, not just IBS. Because of this, researchers are now studying how the FODMAP diet can help in other conditions, including inflammatory bowel disease and chronic diarrhoea in older adults.
There’s also emerging evidence showing it may be helpful in endometriosis-related gut symptoms, infant colic (via the mother’s diet) and people living with functional dyspepsia (ongoing digestive discomfort).
The FODMAP diet can be a powerful tool for understanding and managing your digestive symptoms, but it’s not a one-size-fits-all solution. It’s best to try it after your doctor has ruled out other serious gut conditions such as inflammatory bowel disease, coeliac disease, or bowel cancer.
If you’ve been diagnosed with IBS or experience ongoing digestive issues, the FODMAP diet, when followed under the guidance of a health professional, may be just what you need to finally understand what your gut is trying to tell you!
Feature image: iStock/sefa ozel
The information on this page is general information and should not be used to diagnose or treat a health problem or disease. Do not use the information found on this page as a substitute for professional health care advice. Any information you find on this page or on external sites which are linked to on this page should be verified with your professional health care provider.
Tell us in the comments below: Have you ever been on a FODMAP diet? Was it difficult to stick to?
Read more about gut health:
